Emergency-department (ED) overcrowding is common in countries across the globe. Patients must often wait hours before being seen by a doctor and far longer before being transferred to a hospital bed. The result is not merely inconvenience but rather a degradation of the entire experience—quality of care suffers, patients’ safety is endangered, staff morale is impaired, and the cost of care is increased.
Many hospitals have tried to reduce ED wait times, but their efforts usually fail to produce sustainable results, for two reasons. The first is the narrowness of most performance-improvement programs, which focus solely on the ED. Many of the factors that contribute to ED overcrowding occur in other parts of the hospital and thus are beyond the department’s control. Hospitals are complex, high-stress systems that require significant cross-departmental and cross-role coordination at all times. Even something as seemingly simple as transferring a patient can require the involvement of six to ten clinical and nonclinical staff members. Therefore, the only way to make substantial operational improvements in one part of a hospital is to implement corresponding changes in other areas.
The second reason that many ED-improvement programs do not produce long-lasting results is that they focus only on processes, not staff attitudes. If the changes are to be sustained, the staff must be willing to part with tradition and to collaborate across physical and organizational divides. The hospital’s culture must enable teamwork. Creating this type of culture is, in many ways, the most difficult part of improving ED performance.
Our work with hospitals in multiple parts of the world demonstrates that substantive, sustainable improvements in ED performance can be achieved: average wait times can be lowered by one-third or more, for example, often within a few weeks.1 There is no single “right” approach that can be applied at every hospital, but certain elements are essential for success. Although the performance-improvement program can begin with “quick wins” in the ED, it must also include the wider hospital organization. And significant effort must be put into a cultural shift: the staff must come to understand how seemingly small changes in their actions can improve patient care in other parts of the hospital. To reinforce this cultural shift, the hospital must refine its performance-management systems and enhance its staff’s capabilities to ensure that both buttress the improvement program. Leadership is also crucial: the hospital’s CEO and senior executive team must visibly support the program, and clinicians at the front line of care delivery, especially doctors, must champion the necessary changes.
A performance-improvement program of this type can also be implemented at the health system level to reduce wait times in multiple EDs. This approach can be particularly helpful, for example, when all the EDs in a city are overcrowded.
The limits of quick wins
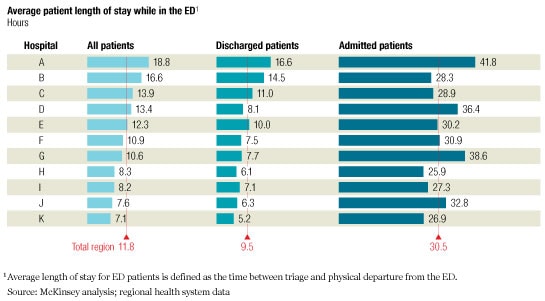
The consequences of ED overcrowding can be profound. Some severely ill patients may be forced to wait too long for treatment, and their condition may worsen as a consequence. Patients with less severe illnesses may leave without being seen by a doctor, only to return later with a more complicated condition. Patients awaiting hospital admission may have to “board” in the ED, lying on gurneys in hallways for hours or days (Exhibit 1). As the overcrowding gets worse, ambulances may have to be diverted to other EDs, the staff may start to feel overwhelmed, and patients’ problems may be overlooked in the general confusion. In addition, costs rise as the efficiency of care diminishes.
ED length of stay
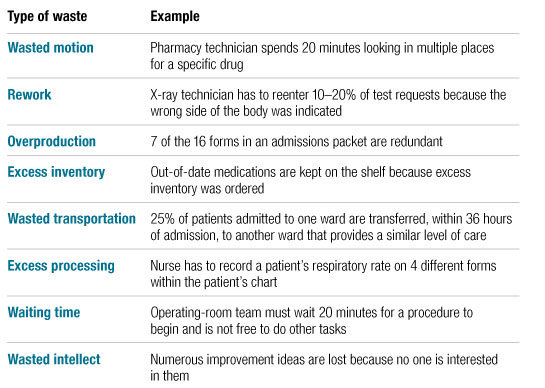
The problems can be alleviated through the application of “lean” principles borrowed from manufacturing. (For more information about them, see sidebar, “How lean principles can transform ED care delivery.”) For example, streamlined triage and registration procedures can minimize the unnecessary administrative work that burdens nurses. Better matching of staff levels with typical patient volumes can prevent patients from being left in the ED because no porters are available to transport them to the wards.
The changes that have the greatest impact vary, depending on the specific challenges a given ED faces. A thorough investigation should therefore be conducted to identify the most important bottlenecks; at the same time, certain “no regrets” changes can be implemented quickly in the ED to drive short-term impact. At one hospital we worked with, for example, the introduction of a fast-track system for patients with low-acuity conditions shortened average wait times by one-and-a-half hours within one week.
These quick wins are important. They provide immediate relief to the ED staff and send a strong signal that change is possible. As a result, they help build support for the improvement program. However, the quick wins offer only limited relief because they do not address the primary causes of ED overcrowding.
Furthermore, an improvement program that focuses on the ED alone might not reduce the overall burden of work; instead, it might inadvertently shift that burden to the inpatient side—a more costly and lower-quality solution. An end-to-end transformation of multiple hospital procedures is required for long-term success.
A hospital-wide transformation
At many hospitals, the primary causes of ED overcrowding include four factors over which the ED staff has no direct control: a lack of free inpatient beds, a lengthy and sometimes convoluted admission process, difficulty getting timely consultations from non-ED physicians, and difficulty getting diagnostic procedures scheduled and results returned. Correcting these problems requires an end-to-end transformation of multiple hospital processes, which can also be accomplished by applying lean principles.
A lack of free beds, for example, prevents admitted patients from being transferred to wards in a timely and efficient manner; as a result, they must board in the ED while beds are found. Resolving this problem rarely requires a hospital to build new wards. More efficient discharge processes—designed to eliminate the unnecessary delays that inappropriately extend length of stay—are usually sufficient to alleviate capacity constraints (Exhibit 2). Some of the process changes needed to speed discharges are quite simple: having doctors write discharge orders earlier in the morning, for example, or having housekeepers clean the beds more quickly once they are vacant.
Expediting admission
Getting the staff to adopt desired behaviors, such as the ones just described, is more difficult, because it requires a shift in mind-sets: the staff must see the connection between their actions and ED overcrowding and understand how changing their behavior can improve patient care. Visual signals can be used to encourage the mind-set shift and reinforce the desired behaviors. For example, signs can be posted in each inpatient unit to remind the full interdisciplinary team of the estimated number of days until each patient’s discharge; the signs encourage the team to make sure that all necessary tests are ordered and that the patients’ families (and, in many health systems, social services) are notified before the day of discharge.
Other process changes may require new support structures or skills. For example, discharge procedures can be expedited if the nursing staff develops checklists to ensure that all appropriate steps are taken and all paperwork is filled out before a patient is ready to be sent home. The streamlined procedures not only enable earlier discharges but also permit the nurses to spend more time on patient education. A daily, early-morning “bed meeting” or a Web-based report available to all staff members can increase collective awareness about bed availability.
Once the beds are freed up, the next step is to get ED patients into them as soon as possible. A streamlined transfer process that includes faxed or electronic transmission of a patient’s records from the ED to the ward can help enormously in this regard. Designating one ED nurse as the equivalent of an air traffic controller can also help. This “flow nurse” can alert others in the hospital whenever backups in the ED are starting to build. Bed assignments can then be made in real time—as soon as another patient is discharged, rather than after the bed is cleaned. (The transfer and bed cleaning can be performed simultaneously.)
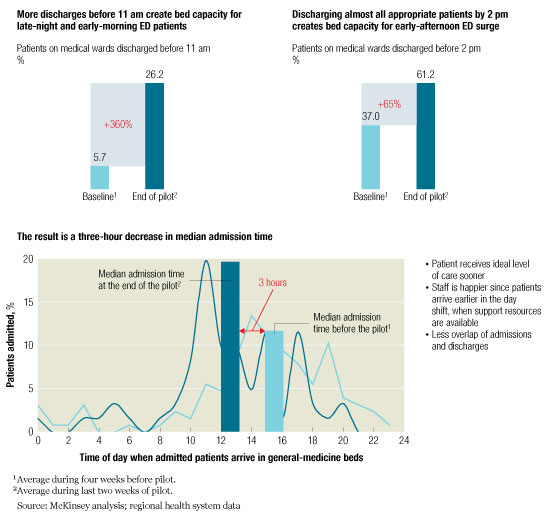
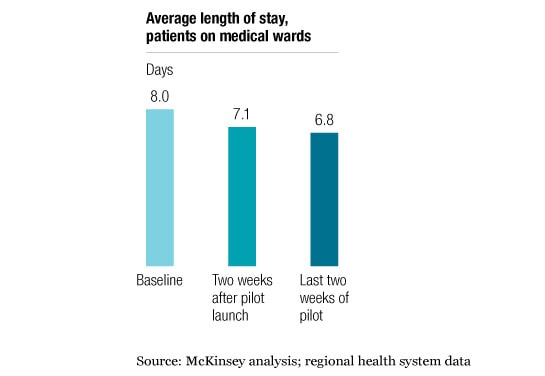
Similar types of changes, also based on lean principles, can be used to streamline admissions, make consultations easier, and increase capacity in the radiology department and diagnostic labs. In most cases, the changes can be implemented inexpensively; they do not typically require new staff positions, unplanned capital expenditures, or significant additional operating resources. But their impact can be profound. One hospital implemented a 14-week performance-improvement program because it was facing a 10 percent increase in the number of patients who came to its ED each year. The program enabled the hospital to double the percentage of patients discharged by 11 AM. As a result, average length of stay decreased by 1.2 days (Exhibit 3), and the number of patients who could be transferred from the ED within eight hours more than doubled. As the hospital’s processes became more efficient, patient safety, patient satisfaction, quality of care, and staff morale rose. The net impact of these changes is that the ED can now comfortably handle 30 percent more patients than before, with the same physical infrastructure and level of resourcing.
Shorter length of stay
Ensuring that changes are sustained
Many hospitals have achieved strong, rapid results by implementing the operational improvements just described. They have found, however, that it can be difficult to get the changes to stick. Cognitive psychology helps explain why: human beings do not make decisions or modify their behavior based on purely rational factors; thus, change programs based solely on those factors are unlikely to succeed.2 Health professionals pride themselves on their scientific rationality, but if their long-term patterns of behavior are to be altered, their beliefs and emotions (their altruistic desire to provide better patient care, for example) must also be engaged. This is the only way to effect a permanent change in the hospital’s culture. A clear message carefully communicated to the staff can begin the process of cultural change; the shift can then be reinforced by improving the staff’s capabilities, strengthening the hospital’s management infrastructure (the formal mechanisms it uses to monitor performance), and providing strong, visible leadership from the hospital’s senior executives and key clinicians.
Communicating to change culture
The long-term success of any performance-improvement program depends on whether the clinical staff is willing and able to change its behavior. It is highly doubtful that employees will change if they think that the improvement program is designed simply to save money (a purely rational argument). But if staff members understand that the program’s primary goal is to improve patient care—and that an ancillary benefit will be a better work experience for them—they will be much more likely to embrace the need for change because their beliefs and emotions will be engaged. Thus, communication is a crucial component of the improvement program.
The communication plan begins with a clear, inspirational message from the hospital’s CEO and executive-management team, underscoring the need for cultural change. General messages we have found to be effective include “Be the change you want to see” and “We can’t solve problems using the same thinking we used to create them.”
In addition, the program’s specific goals must be communicated clearly: improved patient safety, higher quality of care, greater patient satisfaction with treatment, and a better work environment, for example. Both the inspirational message and the program’s goals should then be conveyed to the staff regularly through a variety of formats, including town hall meetings, intranet articles, e-mails, and cafeteria displays. Communications should also make clear that the performance-improvement program is one of the hospital’s top priorities for the coming year.
Before the program begins, surveys and focus groups should be conducted to gauge the staff members’ attitudes, discover the specific issues that are most likely to resonate with them, and identify the barriers most likely to hinder change. The questions asked should stress both the positive (“What strengths can we take advantage of to improve?”) and the negative (“What’s wrong?”). At this stage, listening is critical—even the best communication plan will fail if the information it conveys is not something the staff cares about.
Communication remains important throughout the performance-improvement program. Initially, the staff may be uncomfortable with a lean transformation; as clinicians, they usually adopt new procedures only after the procedures have been proved worthwhile through a lengthy, rigorous process, such as a clinical trial. The more informal, iterative approach used during a lean transformation—designing and piloting solutions, and then rolling out the ones that work well—may therefore strike the staff as less scientific. But the rapid results that can be achieved are often enough to convince them of the benefits of the process. Thus, the program’s successes should be communicated throughout the hospital. The staff’s commitment to change will increase as they learn of the program’s successes, and the needed cultural shift will take place.
Increasing staff capabilities
Education becomes increasingly important once the program is under way. Many staff members may not have the skills needed to identify problems, develop solutions, or ensure that the solutions are sustained. Key staff members should therefore be trained in a variety of skills—not only lean skills, such as process mapping and root-cause analysis, but also how to collaborate, build team trust, and influence others. These staff members can then become role models and coaches for others in the organization, helping them to improve their own capabilities.
In some cases, one-on-one education may be needed. For example, doctors who wait till the late afternoon to write discharge orders may not realize that they are preventing ED patients from being transferred to inpatient beds. By gathering data on each doctor’s typical discharge times, a hospital can identify outliers (the doctors with the latest discharge times) and then use the data to discuss with them how a change in their behavior could improve overall patient care.
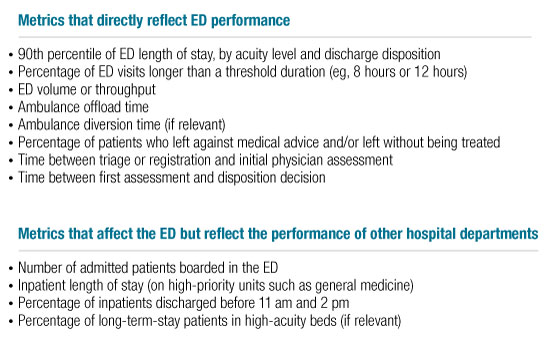
Managing performance well
To sustain the impact of an improvement program, the hospital must clearly define its new operational accountabilities (who is responsible for doing what in the new system), as well as the performance metrics that will be used to determine how well it is achieving its goals. The clinical staff should be closely involved in these decisions; it is much easier for people to accept changes to their jobs and ensure that the changes are sustained if they have had a say in what the changes are. For example, one hospital consulted not only its department heads but also its frontline staff before deciding on the 12 performance metrics it would use to gauge the success of its efforts to reduce ED overcrowding (Exhibit 4). It found that both the staff in the ED and the staff on the inpatient wards had a strong commitment to patient safety and that both groups felt that patients were endangered if they had to board in the ED for hours or days. Thus, both groups recognized the importance of using the number of ED patients waiting for inpatient beds as a performance metric, and both groups were highly motivated to keep that number to a minimum.
Performance metrics
However, even the best metrics will have only limited impact unless the results are visible to all and reviewed regularly during performance discussions. A scorecard delivered by 8 AM each morning can inform all staff members of how many beds the hospital has freed up in recent days and whether it has suffered any blockages in specialized units, such as the ICU; the scorecard can also alert them to what they should expect that day (anticipated discharges and planned admissions, for example, and the number of people still awaiting transfer from the ED). If the scorecard suggests problems, the frontline managers can discuss the results with the staff, determine why the problems arose, and set up plans to correct them (if possible) that day. Midlevel managers can regularly review the results with the frontline managers so that they can identify and resolve the problems that cannot be easily corrected by the frontline staff. The senior executives can monitor the scorecards regularly and hold the midlevel managers accountable for delivering the desired results.
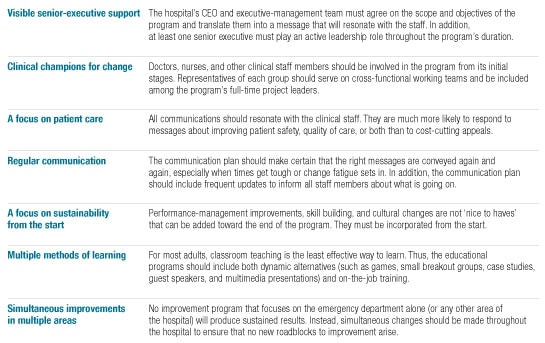
Providing effective leadership
No improvement program can succeed without leadership. At hospitals, two forms of leadership are crucial: senior-executive support and the involvement of key clinicians. The hospital’s CEO and executive-management team must do far more than develop a message to convey to the staff. At least one of them must play an active leadership role in the program throughout its duration. Furthermore, every senior-executive meeting should include a review of progress against the program’s objectives. This high level of senior-executive involvement can be signaled to the staff in multiple ways. One executive we worked with called frontline managers whenever she spotted a recurring problem in the daily scorecards. Another executive held weekly review meetings with midlevel managers. Public celebrations of success can also be effective. A compliment from the hospital’s CEO not only underscores the hospital’s commitment to change but also makes the clinical staff feel that their contributions toward improved patient care have been recognized.
Clinician leadership is also critical to convincing the frontline staff of the need for change. Some clinicians should therefore assume the role of champions for the improvement program by adopting best practices themselves and encouraging their colleagues to do likewise. Given their position in the hospital hierarchy, doctors should play a prominent role, but they should not be the only change champions. Nurses and other health professionals should also be involved.3
Other factors that are important for the success of the improvement program are listed in Exhibit 5.
Key success factors
Achieving results system-wide
Although many performance-improvement programs are carried out one hospital at a time, it is also possible to transform multiple hospitals within the same network or health system as part of a single improvement program. A multihospital approach is particularly helpful when the challenges confronting the network or health system go beyond the four walls of any one hospital. (For example, if long wait times are common in all EDs in a city, then the performance in each ED must be enhanced or access to services will be unequal.) In this situation, the overall goals of the transformation—the substantial improvements that will be made at all hospitals—are established system-wide, but the solutions are tailored to the needs of each facility.
The program is set up so that the hospitals’ participation in the program is staggered. Initially, only a handful of hospitals are included, under the assumption that they will become the reference cases for the system as a whole. As these hospitals undergo the work required to identify the root causes of overcrowding in their EDs and develop appropriate solutions, they are encouraged to share their findings with one another. This helps ensure that, to the extent possible, the solutions that will be piloted are consistent. Once implementation of the solutions begins, the hospitals must also put in place the necessary performance-management improvements and communication/educational programs needed to ensure that culture and capabilities are changed.
A larger set of hospitals is included in the second wave; these hospitals begin the transformation process once implementation at the first set of hospitals is well along. This way, the second set of hospitals can take advantage of the lessons learned by the first set and thus begin implementing proven solutions. If the health system is large enough, the performance-improvement program can be designed to include a third and even a fourth set of hospitals.
When a performance-improvement program is implemented system-wide, it is important that all of the system’s managers use a consistent set of metrics to gauge how the hospitals are doing. These metrics will generally include some of the scorecards the clinical staff uses to monitor results within each hospital, as well as additional measurements designed to assess system-wide achievements. Of necessity, the scorecards used in this type of program will not be as customized as they would have been if they had been developed for a single hospital. But this disadvantage is offset by the fact that the hospitals have the opportunity to learn from one another.
This type of system-wide improvement program can achieve substantial results. One Canadian city opted to transform 13 of its hospitals at once. Within half a year, it had lowered the average wait time in its EDs by almost 20 percent and reduced admission delays by 34 percent. In addition, the number of patients who had to wait in the ED overnight was cut drastically.
At many hospitals, ED overcrowding is a symptom of other problems. Thus, it can signal the need for changes that, if properly implemented, can improve patient care, raise staff morale, and lower costs—not only in the ED but throughout the hospital.