Despite improvements in recent years, the health of the vast majority of sub-Saharan Africans remains in jeopardy. The figures are sobering. One in six children born in the region today will die before age five. African women face more than 100 times the risk of maternal mortality than do women in the developed world. And the average life expectancy in sub-Saharan Africa is a mere 51 years. Sadly, most countries in the region appear unlikely to meet the United Nations’ Millennium Development Goals for health,1 let alone to address significant chronic issues beyond their scope.
The fundamental problem is a pervasive lack of access to primary health care. Conservative estimates suggest that four in ten people in sub-Saharan Africa have no access to medical facilities or personnel. Our experience in the region suggests that the actual figures are often much higher. Moreover, because of Africa’s vast distances and large rural populations, solving its access problem using only traditional clinics staffed with doctors and nurses would be prohibitively expensive and require decades to accomplish.2 Meanwhile, millions of Africans would continue to suffer from diseases that are relatively simple to prevent, treat, and cure.
This need not happen. Our work in recent years suggests that a combination of three delivery approaches could catalyze Africa’s health systems and boost access across the continent, thus dramatically improving the lives of its people. The keys are to employ community-based health officers who would provide essential primary care at the village level, to adopt mobile phone–based “telemedicine” approaches that connect health officers and rural patients with specialized care, and to create networks of mobile health clinics that transport diagnostics and other technologies to remote places. Together, these approaches could quickly save many lives at relatively low cost—about $2 to $3 per person a year, compared with about $8 for traditional clinics.
No access
Access to primary care drives health outcomes. Here’s how: quality access brings treatment and prevention; with treatment and prevention comes education; and with education comes demand. Greater demand for health care, in turn, creates more opportunities for successful and timely treatments that boost demand still further. All of this leads to healthier populations and saves lives.
This cycle is broken across much of sub-Saharan Africa, however, since access to health care is limited or nonexistent. Only 60 percent of the region’s population has even nominal access to health facilities, and the effective figure is often much lower after you factor in the number of doctors, actual access to drugs and equipment, and the productivity of health workers. In Tanzania, for instance, fully 80 percent of the people will never see a doctor in their lifetimes.
To see what might be done, we studied the experience of eight countries3 that have improved on more than one of the United Nations’ Millennium Development Goals for health. Along the way, we interviewed upward of 100 health experts, including African health ministers, academics, specialists from health organizations, and representatives of donor agencies. Notably, we found that each of the eight countries (regardless of income level, geography, or political system) had succeeded by delivering a thorough yet pragmatic range of primary-care services4 to the “last mile” in rural areas.
Encouraged by what we learned, we next looked for novel ideas that might extend these successes. The effort led us to examine 100 or so delivery methods being explored by private, public, and nonprofit groups around the world. From these, we identified the three most promising approaches for Africa.
A new model
While there is no “silver bullet” solution, our work suggests that a model combining local health officers, telemedicine, and, where possible, mobile clinics could help African countries leverage their existing health systems to scale up access to primary health care quickly, effectively, and cheaply. While the model’s individual components aren’t new, together they could help revolutionize health care in African and other low-income countries.
Local health officers
Africa suffers about one-quarter of the world’s burden of disease yet has barely three percent of its health workers. By complementing standard medical doctors with less intensively—though professionally—trained local health officers who serve their home communities, African countries could dramatically improve access to health care. Several practical lessons emerged from our research.
-
Successful programs hire local women as health officers whenever possible. Rural women are perceived as more trusted (and trustworthy) than men by other rural women, and women are already the focal point of many health initiatives, including reproductive ones. While an ideal candidate would be well educated, health officers need only be literate, with a primary education. Countries that have tried to relocate more skilled urbanites to rural areas have struggled both to hire and retain them.
-
Training will vary according to the specifics of a country’s program but should include about 9 to 12 months of formal instruction (classroom and field work) paired with practical apprenticeships to build comprehension, confidence, and independent work habits. Supplemental training is essential. In Bangladesh, for instance, BRAC5 complements its basic training with monthly refresher courses to keep health workers current on best practices in treatment and prevention, as well as to teach new skills.
-
Health workers should have manageable territories—roughly one health officer for every 1,000 to 1,500 people. This ratio ensures that workers can visit patients regularly to monitor them, check compliance, and follow up over time. Bigger territories jeopardize a worker’s ability to serve and build trust with patients.
-
Local health officers must be paid, with compensation ranging from perhaps one-sixth of an average nurse’s salary to 125 percent of the country’s average salary. Volunteer models suffer retention problems and are unlikely to be sustainable. Indeed, Ethiopia’s decision to pay its health extension workers (after initially treating them as volunteers) helped it add 30,000 of them in just five years.
-
Health services should be focused enough to be manageable and affordable yet broad enough to cover a range of essential needs. These will include first aid, basic preventive and diagnostic services, the distribution of materials (say, nutritional supplements or condoms), and essential curative care—as well as the monitoring and, occasionally, treatment of chronic conditions. If the services provided are too narrow, patients will ultimately disregard them. Furthermore, services must be offered at low cost. Small out-of-pocket costs for drugs appear to be bearable, but charging higher sums for services, drugs, and other supplies appears to be impossible on a large scale, at least today.
-
Programs should aspire to an eight-to-one ratio of health workers to supervisors. At these levels, a supervisor can accommodate often lengthy travel times yet still meet with workers at least two to four times a month. In our experience, this level of contact gives health workers enough time to sharpen their skills and even to start viewing their positions as promising careers. (Our work in Tanzania suggests that career development can be more important than financial considerations to health officers.) Best-practice programs will focus on supervision and performance management—using checklists and other simple tools to keep guidance fair and thorough—while striving to create opportunities for professional growth.
By applying these best practices and employing groups of local health officers, African countries could address the bulk of the most important clinical conditions they face. Furthermore, meeting this goal would require just a single local health officer per every 1,000 to 1,500 people, at a cost of about $1 a year per capita. This staffing level would give patients more than three meaningful interactions a year with trained medical personnel—a dramatic improvement over the status quo.
Telemedicine
Once African countries establish a critical mass of local health officers to serve as first responders, they could harness the power of mobile telephony to dramatically increase the scope of more extensively trained health workers, such as doctors and nurses. The technology is readily available. In fact, most people in sub-Saharan Africa already have access to mobile phones through friends, family, or group sharing agreements. Moreover, typical African countries have 2G and 3G data service and coverage rivaling that of the United States, often with better reception.
A successful model, we believe, would employ urban call centers staffed by clinical officers,6 nurses, and doctors. Instead of serving patients directly, these centers would act as hubs that increase the impact of local health officers by providing them with advanced clinical support (exhibit)—for example, in making diagnoses in the field. (Mozambique has successfully used mobile phone–based diagnostic tools for this purpose.)
A district-level call center staffed with doctors and nurses functions as a support hub that makes local health officers more effective.
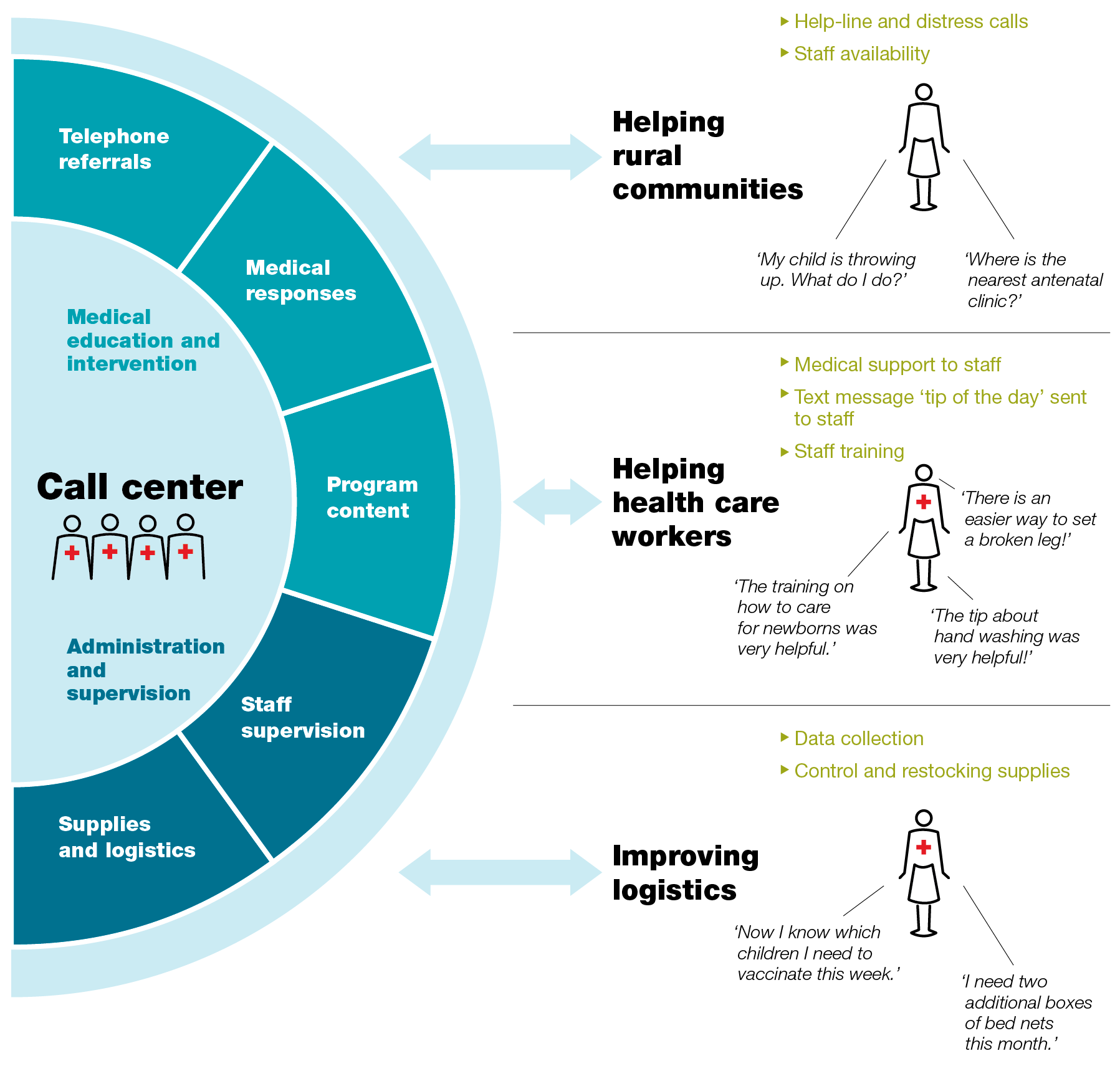
Just as important, call centers could also support the personalized training and supervision of health workers by giving them access to more skilled advisers than they could get locally. Local health officers could submit medical data and updates to a call center on an ongoing basis (for example, by voice or text message), and supervisors could follow up with 30-minute calls every one or two weeks. The combination of better data and better interactions with supervisors could help health workers improve the quality and timing of their interventions (say, by creating improved vaccination schedules for a community). Supervisors could manage the performance of local health workers more effectively—a common challenge in systems using them in hard-to-reach rural areas. All this comes at quite a low cost. Assuming one check-in a week, a supervisor could support 50 or 60 health officers; biweekly check-ins would double the span of control. Such call centers, which would cost about $0.75 a year per person, are affordable.
Private models serving patients directly will be increasingly viable, as well. While no business model has won the race to deliver telemedicine at scale in Africa, some promising experiments suggest what’s possible. In Mexico, for instance, MedicallHome (partly owned by the telecom provider Telmex) successfully provides over-the-phone medical advice and triage services to about one million households (five million people) for a flat $5 a month each. The company, which fields about 90,000 calls a month, uses triage protocols developed by the Cleveland Clinic, a leading US medical institution, to help its doctors serve patients quickly and effectively. Many cases are resolved by doctors over the phone and don’t require further consultation or emergency care.
Mobile health clinics
The third piece of the puzzle is the use of mobile clinics to bring diagnostic tools, medicines, and supplies to local communities where possible. Mobile clinics have long served this function. In recent years, however, various organizations have begun employing them at scale. This suggests that they could play an important role in maximizing the reach of local health officers, while further lowering the transport barriers that keep many Africans from receiving care.
In India, for example, the nonprofit Health Management and Research Institute deployed 475 mobile clinics across Andhra Pradesh in just one year and is using them to improve medical coverage for the state’s massive rural population. Turkey’s government has used mobile clinics to give large portions of the country’s rural population greater access to about 80 medical services. Egypt’s government uses truck convoys to transport temporary hospitals around the country. Comparable experiments are under way elsewhere in India, as well as in Namibia, Nigeria, and other African countries.
While no single best-practice template will work across Africa—budgets, infrastructure constraints, and terrain vary too dramatically—our research suggests that successful models will embody several characteristics.
-
Smaller is generally better: vans can cover more of Africa’s diverse terrain and poor roads than larger vehicles can. The vans should be equipped with coolers to transport refrigerated vaccines, medicines, and lab samples to and from faraway health clinics. They should also have a bed to treat patients and to accommodate a doctor or nurse-practitioner on multiday journeys.
-
The vans can focus on providing care for chronic conditions and more complex follow-up interventions (say, antenatal care). They should play a primary role in providing direct support for health officers’ activities, as well. A van’s supplies will therefore include test kits, basic medicines, and some equipment (higher-end gear like ultrasounds would be ideal). Services could include education and awareness, screening, diagnosis, treatment, the delivery of supplies, and supplemental training for local health officers.
-
Routes must be chosen carefully so that each community can receive a visit at least every four weeks. The key is to minimize travel time and maximize treatment time. Health clinics can serve as a natural base of operations and resupply for mobile journeys, which might take two or three days and cover a number of villages. Whenever possible, trained schedulers in call centers should coordinate scheduling, with input from local health officers.
-
Routes must be well advertised and timetables kept so that patients are properly screened and paperwork doesn’t eat into treatment time.
-
Finally, maintenance and running costs must not be overlooked. When mobile clinics fail to show up in villages because of breakdowns, patients quickly become disillusioned and a program’s potential declines.
Despite the versatility of mobile clinics, their operating costs are quite reasonable when programs are designed to supplement the work of local health officers (through monthly visits, for example). In fact, we estimate that a mobile clinic staffed by two nurses would cost less than $0.75 per person a year in most African countries.
The way ahead
The model we propose would deploy a significant—but feasible—level of resources in areas that are now poorly served. A rural region of one million people, for instance, would require 700 to 1,000 village health officers, a call center with 40 to 50 clinicians (a mix of clinical officers, paramedics, nurses, and doctors to support inbound calls from village health officers and the general public), 10 to 15 supervisors responsible for outbound planning and follow-up calls to village health officers, and 20 to 25 mobile clinics, each staffed by one or two nurses. This model would require one-fifth to one-tenth as many nurses and doctors as traditional clinics do. And since nurses and doctors in call centers can be located in major urban areas, where many of them live, the approach is practical given the current distribution of resources.
It’s important that the model we propose would not—and must not—replace Africa’s existing national health systems and infrastructure but should instead help extend their reach by making better use of their doctors, nurses, and other health care workers. Moreover, this is not a “lesser” model for the developing world. In fact, some governments and private entrepreneurs in developed countries are not only introducing telemedicine call centers and mobile clinics but also experimenting with the idea of shifting many tasks to nurse-practitioners.
To make the model work, African governments should start by determining the package of services they can afford and then explore practical ways to deliver them. The private sector will have a significant role, as it is a “natural owner” of some elements (notably call centers) and already plays an important role in delivering health care in Africa. With the right investments, the private sector could do even more.
Finally, assistance and investments from donors will be vital in taking the model to scale, since donors are well positioned to support promising (but subscale) ventures by providing start-up capital and funds to support implementation.
By embracing a model combining local health officers, telemedicine, and mobile clinics, Africa can radically improve access to basic health care and provide essential, life-saving services to its people at low cost. Making the model scalable and sustainable will require significant and concerted efforts from both the public and private sectors. Nonetheless, the goal of radically improving health outcomes in Africa is now firmly within reach.
